What Is Dry Macular Degeneration?
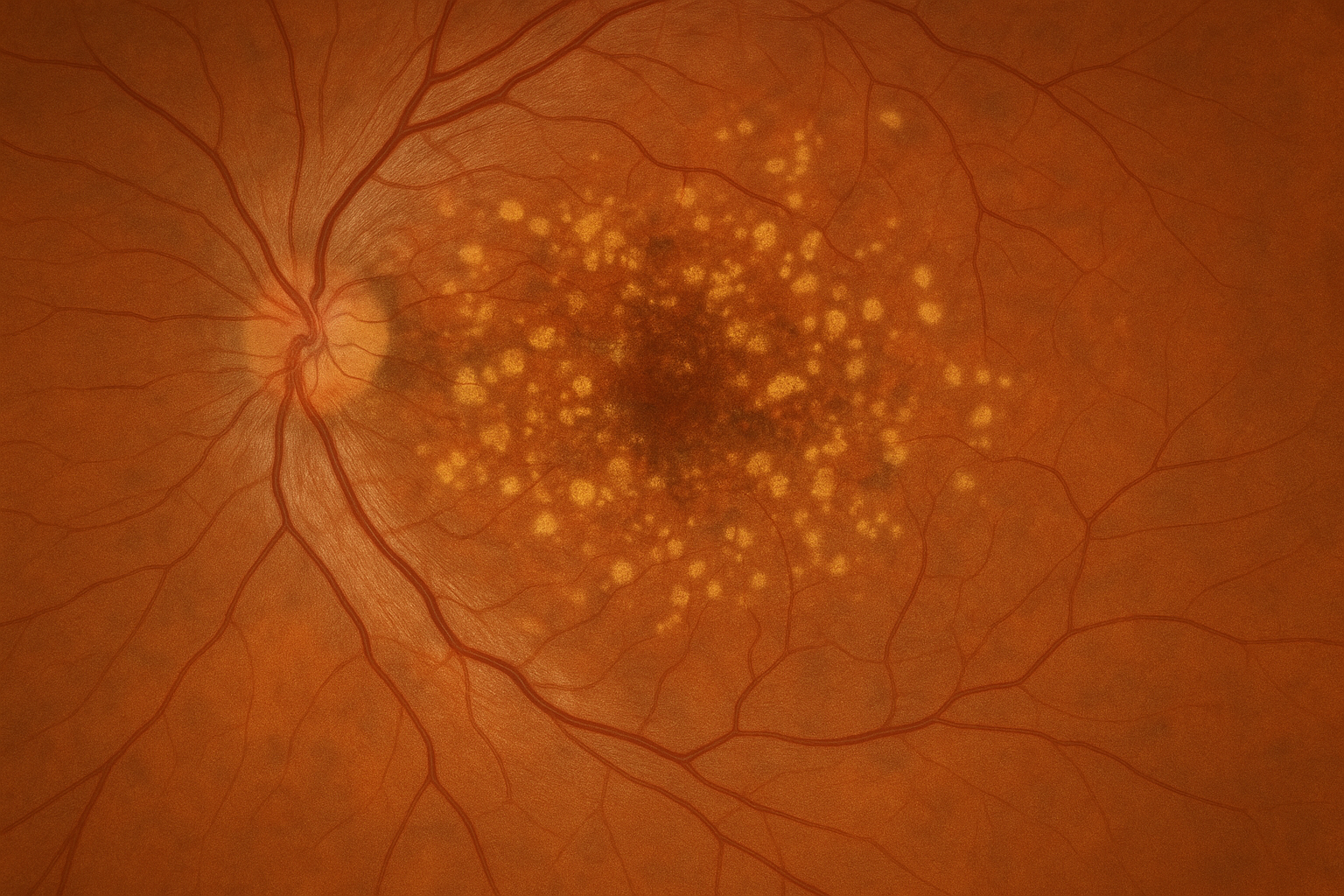
Dry Age-Related Macular Degeneration (Dry AMD) is the most common form of macular degeneration, a progressive eye disease that affects the macula—the central portion of the retina responsible for sharp, straight-ahead vision. Over time, the cells in the macula begin to break down and thin, leading to a gradual loss of central vision.
Unlike the “wet” form of the disease, Dry AMD does not involve bleeding or fluid leakage but still has a significant impact on activities like reading, driving, and recognizing faces.
Why Does Dry AMD Happen?
Dry AMD is primarily age-related and tends to develop slowly over time. While the exact cause isn’t fully known, certain factors can increase the risk:
- Age (most common in those over 60)
- Family history of macular degeneration
- Smoking
- High blood pressure or cardiovascular disease
- Prolonged sun exposure
How Is Dry AMD Treated?
Currently, there is no cure for Dry AMD, but regular monitoring and strategic interventions can help slow its progression and preserve vision. At our clinic, we focus on:
- Routine monitoring to track disease progression and detect any signs of conversion to Wet AMD as early as possible.
- Lifestyle guidance such as smoking cessation, UV protection, and maintaining a diet rich in leafy greens, fish, and antioxidants.
- Supplementation with the AREDS 2 formula for patients with intermediate to advanced Dry AMD. This specific combination of vitamins and minerals—including vitamin C, vitamin E, lutein, zeaxanthin, zinc, and copper—has been clinically proven to reduce the risk of the disease advancing to later stages.
We are committed to helping patients understand their condition, manage their risk factors, and preserve their vision through proactive, personalized care that includes the latest evidence-based approaches like the AREDS 2 formula.
How Do We Test for Dry AMD?
Our clinic uses advanced technology to detect and monitor Dry AMD, even in its earliest stages. Key tests include:
- Optical Coherence Tomography (OCT) – This non-invasive scan provides detailed cross-sections of the retina, allowing us to assess thinning, drusen, and other changes in the macula over time.
- Optos widefield retinal imaging – Offers a comprehensive view of the retina to evaluate overall retinal health.
- OCT-Angiography (OCT-A) – Helps ensure that no abnormal blood vessels (which would indicate conversion to Wet AMD) are forming.
- Visual acuity testing and Amsler grid monitoring – Help detect subtle changes in central vision and distortion that may indicate progression.
These tools allow us to closely monitor changes and provide timely updates and recommendations to patients.
