What Is Diabetic Retinopathy?
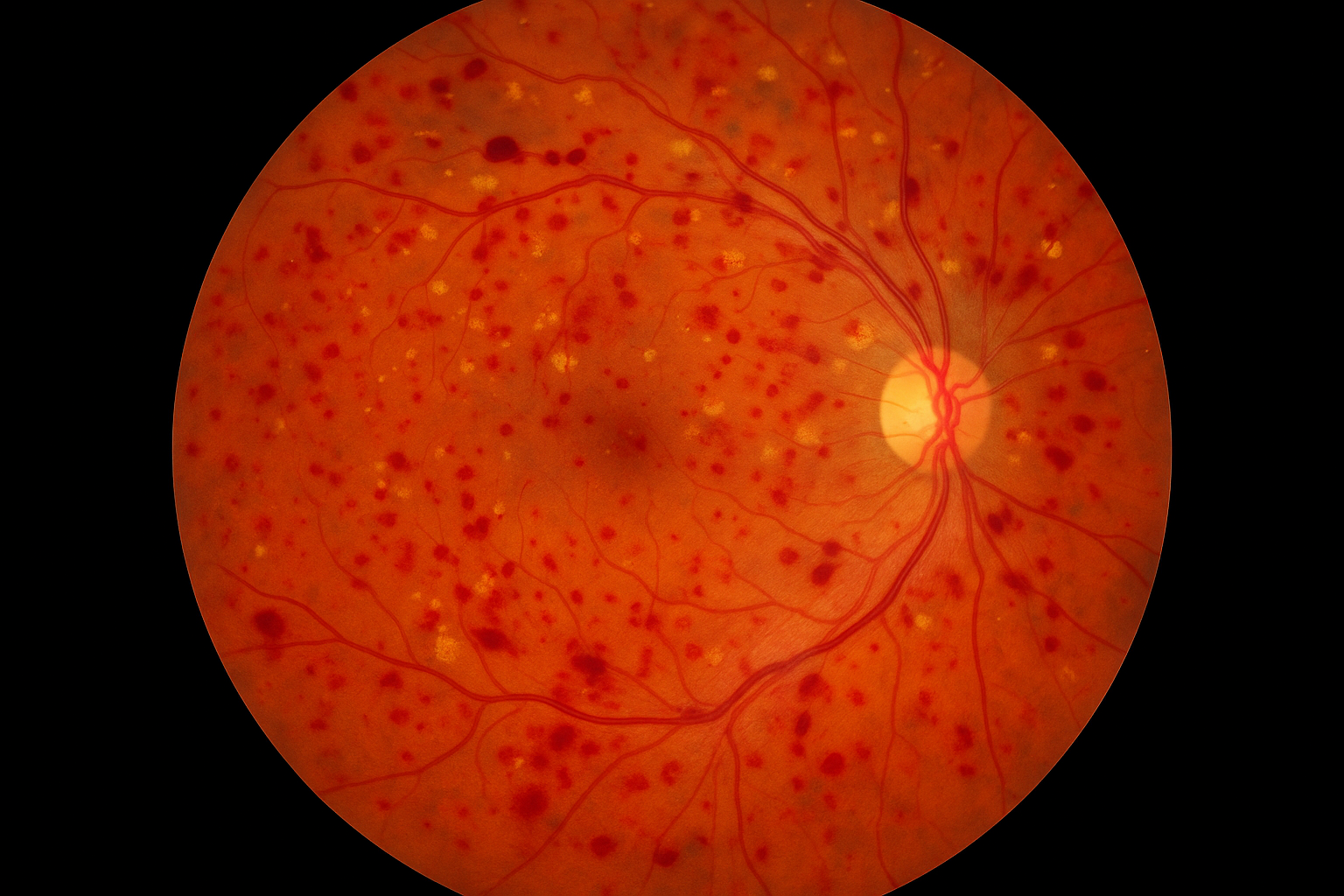
Diabetic Retinopathy is a diabetes-related eye condition that affects the blood vessels in the retina—the light-sensitive tissue at the back of the eye. Over time, high blood sugar levels can damage these small blood vessels, leading to vision problems and, in severe cases, blindness if left untreated.
How Is Diabetic Retinopathy Monitored?
The key to preventing vision loss from diabetic retinopathy is early detection and consistent monitoring. That’s why we work closely with patients and their primary care providers to manage eye health as part of a comprehensive diabetes care plan.
Why Does Diabetic Retinopathy Happen?
When blood sugar remains elevated over long periods, it can weaken and damage the tiny vessels in the retina. This can cause them to leak fluid or blood, close off entirely, or stimulate the growth of abnormal new vessels. Diabetic Retinopathy usually develops gradually and is more likely to occur in people who:
- Have had diabetes for many years
- Have poorly controlled blood sugar levels
- Have high blood pressure or high cholesterol
- Smoke
- Are pregnant while diabetic
How Do We Test for Diabetic Retinopathy?
Our clinic uses advanced, non-invasive imaging technology to detect and monitor diabetic eye disease, even before symptoms appear. Key testing includes:
- Optos widefield retinal imaging, which provides a panoramic view of the retina, allowing us to detect even early signs of vessel damage or bleeding.
- Optical Coherence Tomography (OCT), which offers high-resolution cross-sectional images of the retina to assess swelling, fluid buildup, and retinal thickness.
- Angiography (if needed), to evaluate blood flow and detect leaking or blocked vessels.
- Regular visual acuity assessments to track changes in sharpness and clarity over time.
